Venous Ulcer Treatment Options: Expert Tips for Long-Term Relief
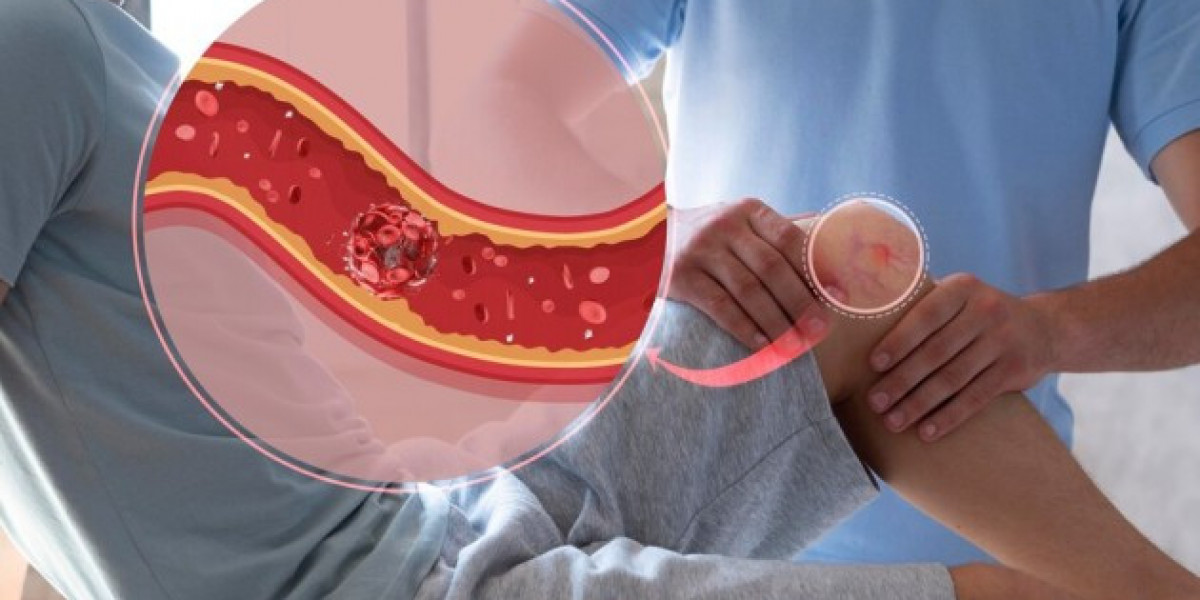
Venous ulcers, often referred to as venous stasis ulcers, are chronic wounds that develop due to poor blood flow in the lower legs. These open sores are not only painful but can also significantly impact a person’s quality of life. While they may take weeks or even months to heal, the right venous ulcer treatment options can help manage the condition effectively and ensure long-term relief.
This comprehensive guide explores the causes, symptoms, and expert-recommended treatments for venous ulcers. Whether you’re currently dealing with one or seeking to prevent recurrence, this article will provide valuable insights to guide you on the path to recovery.
Understanding Venous Ulcers
What Are Venous Ulcers?
Venous ulcers are open sores that commonly occur on the lower legs, especially near the ankles. They result from chronic venous insufficiency (CVI), where damaged vein valves prevent proper blood flow back to the heart. This leads to blood pooling in the legs, increasing pressure, and damaging the surrounding tissues.
Common Symptoms
Identifying the early signs of venous ulcers is crucial for timely venous ulcer treatment. Symptoms include:
Open sores or wounds that fail to heal over time.
Swelling and inflammation in the legs or around the ulcer.
Discoloration of the skin, often appearing red, brown, or purple.
Hardened, thickened, or itchy skin around the affected area.
Pain or tenderness, which may worsen with prolonged standing or walking.
Causes of Venous Ulcers
Several factors can contribute to the development of venous ulcers, including:
Chronic Venous Insufficiency (CVI): The primary cause of venous ulcers, CVI occurs when vein valves are weakened or damaged, leading to poor circulation.
Deep Vein Thrombosis (DVT): Blood clots in deep veins can obstruct blood flow, increasing the risk of ulcers.
Varicose Veins: Enlarged, twisted veins contribute to venous insufficiency and may lead to ulcers.
Obesity: Excess body weight increases pressure on veins in the lower extremities, worsening circulation.
Injury or Trauma: Even minor injuries can turn into venous ulcers if blood flow is compromised.
Understanding these underlying causes is the first step toward effective venous ulcer treatment.
Effective Venous Ulcer Treatment Options
Managing venous ulcers requires a multifaceted approach that combines medical interventions, wound care, and lifestyle changes. Below are expert-recommended treatment options:
1. Compression Therapy
Compression therapy is considered the cornerstone of venous ulcer treatment. It involves applying pressure to the legs to improve blood flow and reduce swelling.
Compression Devices Include:
Compression stockings.
Multi-layer compression bandages.
Pneumatic compression pumps for severe cases.
Compression therapy not only accelerates healing but also helps prevent the formation of new ulcers.
2. Proper Wound Care
Regular wound care is critical to promote healing and prevent infection.
Cleaning the Ulcer: Use a saline solution or gentle cleanser to remove debris and bacteria.
Dressing Options:
Foam dressings for absorbing excess fluid.
Hydrocolloid dressings to maintain a moist environment for healing.
Antimicrobial dressings to prevent bacterial growth.
Debridement: This process involves removing dead or damaged tissue to encourage the growth of healthy cells.
Consistent wound care is essential for any venous ulcer treatment plan.
3. Medications
Medications can play a supportive role in treating venous ulcers.
Antibiotics: Prescribed when there are signs of infection, such as redness, swelling, or pus.
Topical Treatments:
Antimicrobial creams to prevent bacterial infections.
Growth factor gels to speed up tissue regeneration.
Pain Management: Over-the-counter or prescription medications can help alleviate discomfort.
4. Advanced Medical Procedures
For ulcers that do not respond to conventional treatments, advanced medical procedures may be necessary.
Endovenous Laser Therapy (EVLT): This minimally invasive procedure uses laser energy to close damaged veins, improving circulation.
Sclerotherapy: A solution is injected into varicose veins to seal them and redirect blood flow.
Skin Grafting: In severe cases, healthy skin is transplanted to cover the ulcer and promote healing.
Vein Surgery: Surgical removal of damaged veins may be recommended for persistent or severe ulcers.
5. Lifestyle Changes
Incorporating healthy habits can significantly enhance the effectiveness of your venous ulcer treatment and prevent recurrence.
Exercise Regularly: Activities like walking or swimming improve blood circulation and strengthen leg muscles.
Elevate Your Legs: Raising your legs above heart level for 20–30 minutes a few times a day reduces swelling and improves blood flow.
Maintain a Healthy Weight: Losing excess weight eases the strain on your veins.
Avoid Prolonged Sitting or Standing: Take regular breaks to stretch your legs and improve circulation.
Home Remedies to Complement Treatment
In addition to professional care, home remedies can support healing and offer relief:
1. Aloe Vera
Aloe vera is known for its soothing and anti-inflammatory properties.
How to Use: Apply fresh aloe vera gel directly to the ulcer and cover it with a clean dressing.
2. Honey
Honey has natural antibacterial properties that aid in wound healing.
How to Use: Spread a thin layer of medical-grade honey on the ulcer before applying a dressing.
3. Turmeric Paste
Turmeric contains curcumin, which has anti-inflammatory and antimicrobial effects.
How to Use: Mix turmeric powder with water to form a paste and apply it around the ulcer.
4. Coconut Oil
Coconut oil helps moisturize the skin and reduce irritation.
How to Use: Massage coconut oil gently around the ulcer to keep the skin hydrated.
Preventing Venous Ulcers
Preventing venous ulcers is equally as important as treating them. Here are some expert tips for prevention:
Wear Compression Stockings: These improve circulation and reduce venous pressure in the legs.
Stay Active: Regular exercise strengthens your leg muscles and improves blood flow.
Practice Good Skin Care: Keep your skin clean, moisturized, and free from irritants.
Quit Smoking: Smoking damages blood vessels and impairs circulation, slowing healing.
Monitor Your Health: If you have a history of venous insufficiency or varicose veins, schedule regular check-ups with a healthcare provider.
When to Seek Medical Attention
It’s essential to consult a doctor if you experience:
Persistent pain or discomfort in the ulcer area.
Signs of infection, such as redness, swelling, or discharge.
Wounds that do not show signs of healing after two weeks of care.
Timely intervention ensures that your venous ulcer treatment plan is effective and reduces the risk of complications.
Conclusion
Venous ulcers can be a challenging condition to manage, but effective venous ulcer treatment options are readily available. From compression therapy and proper wound care to advanced medical procedures and lifestyle changes, there are numerous strategies to help you heal and prevent recurrence.
By taking a proactive approach to treatment and prevention, you can improve your quality of life and protect yourself from the discomfort and complications associated with venous ulcers. Consult a healthcare professional to develop a personalized treatment plan and take the first step toward long-term relief and healthier legs today!