What are Vitreous Tamponades?
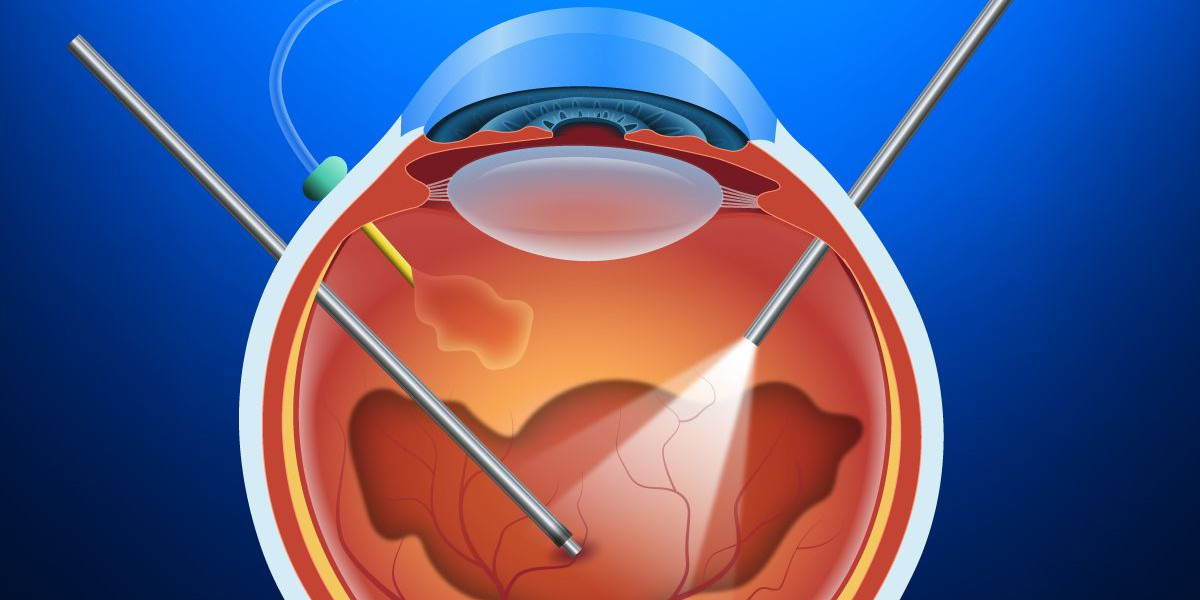
A vitreous tamponade is a substance that is injected into the eye during retinal detachment surgery to help push the retina back into position against the back interior wall of the eye. Vitreous tamponades are used when a gas bubble or oil cannot provide enough support on its own.
Types of Vitreous Tamponades
There are three main types of Vitreous Tamponades used during retinal detachment surgery:
Gas Tamponades
Gas tamponades, such as sulfur hexafluoride or perfluoropropane, are colorless, invisible gases that are injected inside the eye. As the gas is heavier than aqueous humor, it allows the detached retina to settle back into position against the interior wall of the eye. Gas tamponades are typically absorbed by the body within 2-8 weeks after surgery.
Silicone Oil Tamponades
Silicone oil is a viscous, clear liquid used as a long-acting tamponade. It is heavier than water and provides continuous tamponade effect for several months inside the eye. Silicone oil must later be surgically removed once the retinal tears have sealed and the retina has fully reattached itself.
Perfluorocarbon Liquids
Perfluorocarbon liquids are clear tamponades that are heavier than both water and silicone oil. They are used less commonly but provide a longer-acting internal tamponade than gases alone. Like silicone oil, perfluorocarbon liquids must later be surgically removed.
How Vitreous Tamponades Work
During retinal detachment surgery, the vitreous gel is removed from the inside of the eye. Any retinal tears or breaks are identified and treated, usually with cryotherapy or laser photocoagulation to seal them. A vitreous tamponade is then injected inside the eye to push the retina back into correct position against the retinal pigment epithelium layer.
The tamponade agent creates an internal pressure inside the eye that counteracts the tractional forces pulling the retina away from the back interior wall. It also seals any remaining retinal defects to prevent new retinal detachments from forming. As the tamponade is absorbed or removed over time, it allows the retina to re-adhere permanently to the retinal pigment epithelium layer.
Potential Risks and Complications
While vitreous tamponades are generally very effective at treating retinal detachments, there are some potential risks and complications to be aware of:
- Increase in intraocular pressure - The tamponade can temporarily raise eye pressure, sometimes requiring topical eye drops or other measures.
- Cataract formation - Some tamponades, especially silicone oil, increase the risk of developing cataracts over time that may require surgery.
- Corneal decompensation - Rarely, long-term exposure to silicone oil can damage the corneal endothelium resulting in corneal edema.
- Migration of tamponade into adjacent eye structures - In rare cases, the tamponade agent travels into the anterior chamber, vitreous cavity, or other unintended areas.
- Inflammation or infection - As with any intraocular surgery, there is a small risk of post-operative inflammation, infection or endophthalmitis.
- Proliferative vitreoretinopathy - In some cases, the retina may re-detach due to the growth of scar tissue even after successful surgery and tamponade use.
For most patients, the benefits of regaining vision with a vitreous tamponade outweigh these potential complication risks. Close monitoring after surgery is important to catch any issues early.
Outcomes After Vitreous Tamponade Surgery
When used appropriately, vitreous tamponades have a very high success rate of reattaching the retina permanently. Success rates vary depending on specifics of each case and the amount of existing retinal damage, but are generally:
- Around 90% after a single surgery for rhegmatogenous retinal detachments involving retinal breaks.
- Approximately 80-85% after a single surgery for more complex detachments related to proliferative vitreoretinopathy or extensive retinal breaks/tears.
- Even higher success rates of over 95% can be achieved after multiple re-attachment surgeries if needed.
Provided the retina remains fully attached after removal of the tamponade, most patients experience stabilization or improvement of their vision. However, in long-standing or very advanced cases, severe and permanent vision loss may have already occurred prior to surgery. Still, vitreous tamponades offer the best current chance of vision restoration for many retinal detachments when used by an experienced retinal surgeon.
In the vitreous tamponades play an important role in retinal detachment surgery by helping to push the retina back into correct position and preventing re-detachments from occurring as the retina heals. With diligent post-operative monitoring, they provide highly effective reattachment rates and functional vision outcomes for many patients dealing with this challenging ocular condition.
Get This Report in English Language: Vitreous Tamponades
Get This Report in Japanese Language: 硝子体タンポナーデ
Get This Report in Korean Language: 유리체 탐포나이드
About Author:
Vaagisha brings over three years of expertise as a content editor in the market research domain. Originally a creative writer, she discovered her passion for editing, combining her flair for writing with a meticulous eye for detail. Her ability to craft and refine compelling content makes her an invaluable asset in delivering polished and engaging write-ups.
(LinkedIn: https://www.linkedin.com/in/vaagisha-singh-8080b91)